Sannova
To date, the Food and Drug Administration (FDA) has approved about twenty-nine biosimilars1, and the European Medicines Agency (EMA) has approved seventy-seven2 biosimilars3. Given the increased awareness and significance of biosimilars, the FDA is expected to vet and approve even more in coming years.
In fact, the latest Executive Order on Promoting Competition in the American Economy (2021) directly calls for agencies, such as the FDA, to use their regulatory authority to increase patients’ access to biosimilars and generics.
Prior to this order, lawmakers enacted the Biologics Price Competition and Innovation Act (2009) to establish an abbreviated pathway for the approval of biosimilars.
Sponsors must tackle the next big challenge to moving biosimilars forward:
Immunogenicity
The immune response to foreign proteins, represents a critical safety concern for bringing any protein therapy, like recombinant insulin or monoclonal antibodies, to market. Unlike generics drugs, biosimilars are not exact copies of the reference compound. In the same way that people carry specific glycans, which determine their individual blood type in the ABO system and their immune response to other blood types, biologics that share the same primary sequence and perform equivalent functions may differ in their glycans (Akram et al., 2021). As a result, extra care must be taken to analyze not only the functional equivalence of biosimilar candidates to the original, but also to understand the extent to which any structural deviances – like varied glycosylation patterns – might pose immunologic harm to patients.
Multiple case studies have found structural and functional variations in the glycan profile of biosimilars and their originator drug – with functional consequences. For instance, in 2018, scientists demonstrated that the presence of high variability in the glycosylation pattern of rituximab and five approved biosimilars was correlated with differences in their biological activity in vitro (Nupur et al.). Similarly, studies of infliximab biosimilars revealed significant differences in their glycosylation profiles and immunoglobulin receptor binding activity (as reviewed in Duivelshof et al., 2019). Varied glycosylation patterns have been shown to produce significant differential immune responses in patients. For example, an N-glycosylation site in the Fab portion of the heavy chain of cetuximab was implicated in the high prevalence (~33%) of cetuximab-induced anaphylaxis in human subjects; to prevent these types of drug-induced hypersensitivity reactions, scientists have engineered CHO cells or yeast strains in ways that control and optimize glycosylation (Beck, 2011). Consequently, sponsors have generated biobetters, which have an improved safety profile or other desirable qualities, relative to the reference protein (Akram et al., 2021; Beck, 2011).
At Sannova, we can not only characterize the immunogenicity of your target, but we can also provide insight into why a target is immunogenic – enabling sponsors to make necessary modifications in lead development. To do this, we combine electrochemiluminescence (ECL) with high-resolution mass spectroscopy.
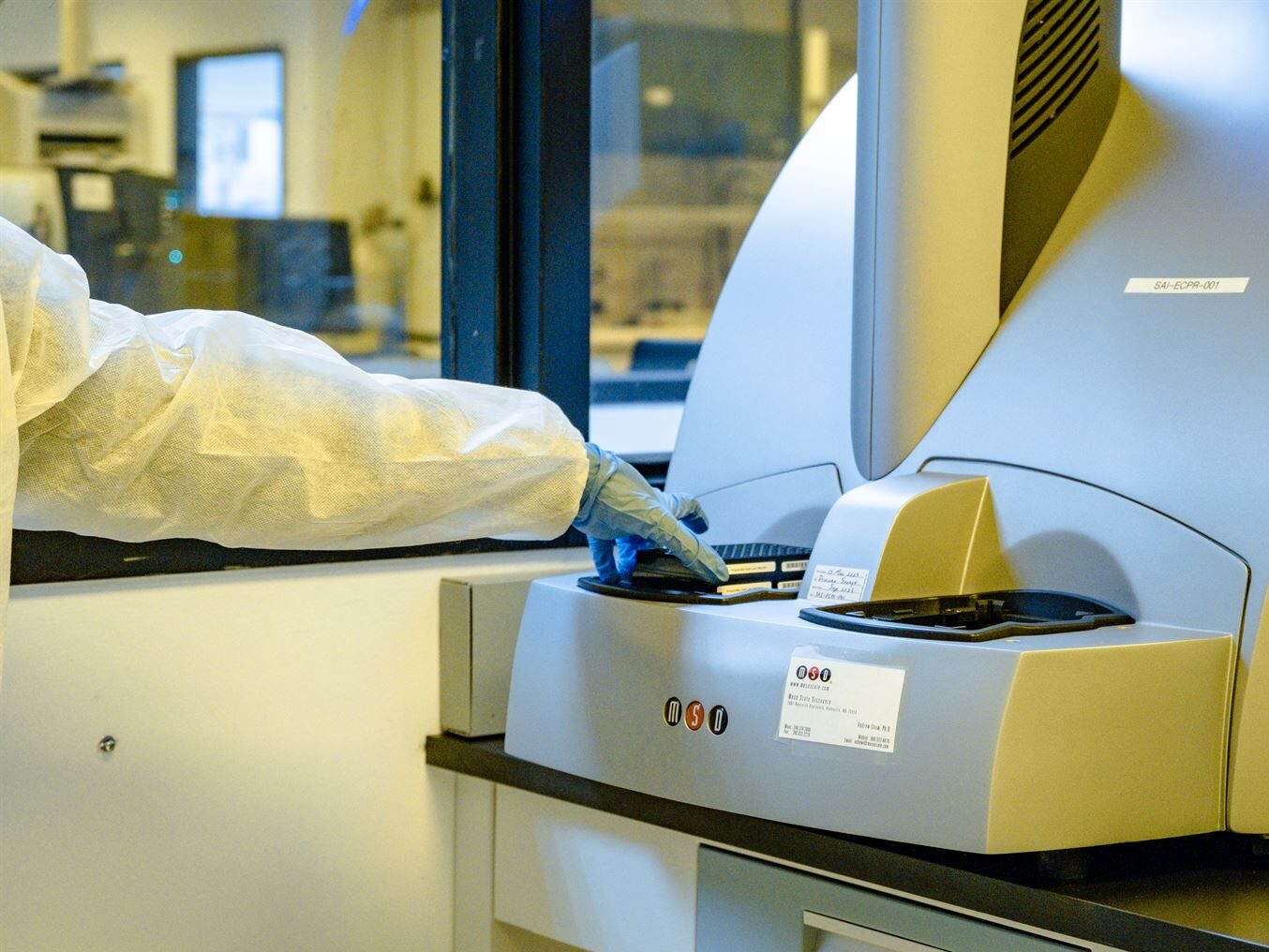
ECL is the gold-standard technique for performing immunogenicity testing and anti-drug-antibody (ADA) assays within the pharmaceutical industry. ECL immunoassays, compared to ELISAs, require far less of the target sample, feature some of the most sensitive detection labels with minimal background issues, and possess the high spatiotemporal resolution necessary for multiplexing several analytes in parallel (Zhang et al., 2019). The Meso Sector S 600 ECL instrument at Sannova, for example, is able to analyze up to 10 analytes per well. If desired, ECL imaging can also be adapted for visualizing and measuring biomarkers or coupled with enzyme-based immunoassays – through existing kits or via methods developed in-house. Researchers are also exploring ECL microscopy as a method for investigating cellular trafficking and membrane transport (Zhang et al., 2019). Despite its varied uses, ECL can only help to determine whether or not a target is immunogenic; another analytical highly sensitive analytical approach must be used to identify the identity and site of the post-translational modifications (PTMs) responsible for any immunogenic activity.
High-resolution mass spectroscopy (HRMS) gives us the power to determine what glycans or PTMs, are present at specific sites of your target molecule. In addition to the N-glycan profiling used by Nupur et al. (2018) to characterize rituximab and its biosimilars, O-glycan profiling is also emerging as an option, though all glycan profiling is non-trivial (Duivelshof et al. 2019). Other relevant posttranslational modifications, such as phosphorylation or lipidation, can also be identified and analyzed using HRMS.
Biosimilars enjoy a unique, accelerated pathway to regulatory approval with the caveat that compounds must be similar enough to the reference drug to be safe and effective. Numerous studies have shown that the glycan profiles of biosimilars differ in ways that have in vitro and in vivo effects on the immune system. Bioanalytical assays such as electrochemiluminescence are routinely used to characterize the immunogenicity of drug targets. In conjunction with techniques such as HRMS, biochemical analysis enables scientists to identify and characterize structural features such as glycosylation, which are key to developing optimal pharmaceutical compounds.
Thus, by using state-of-the-art analytical chemistry techniques to profile glycans and other moieties that underlie immunologic risk, we can partner together to ensure that patients have confidence in the safety, quality and potency, in addition to cost-savings, that biosimilars can provide in the near future. So far, Americans have had access to fewer biosimilars than their European counterparts. But, in the current regulatory climate, sponsors may have a unique opportunity to move biosimilars forward – providing increased options to patients in the US, as well as abroad.
References
- Biosimilar Product Information | FDA (accessed July 13, 2021).
- Of these seventy-seven candidates, some were withdrawn or refused – leaving the adjusted number of EMA biosimilar approvals at 69. See Biosimilars approved in Europe (gabionline.net) (accessed July 13, 2021).
- How the U.S. Compares to Europe on Biosimilar Approvals and Products In the Pipeline | Biosimilars Law Bulletin (biosimilarsip.com) (accessed July 13, 2021).
- Akram, M. S.; Pery, N.; Butler, L.; Shafiq, M. I.; Batool, N.; Rehman, M.; Grahame-Dunn, L. G.; Yetisen, A. K. Challenges for biosimilars: Focus on rheumatoid arthritis. Crit. Rev. Biotechnol. [Online] 2021, 41, 121–153. https://doi.org/10.1080/07388551.2020.1830746 (accessed July 22, 2021).
- Beck, A. Biosimilar, biobetter, and next generation therapeutic antibodies. mAbs [Online] 2011, 3, 107-110. https://www.tandfonline.com/doi/full/10.4161/mabs.3.2.14785 (accessed July 7, 2021).
- Duivelshof, B. L.; Jiskoot, W.; Beck, A.; Veuthey, J. L.; Guillarme, D.; D’Atri, V. Glycosylation of biosimilars: Recent advances in analytical characterization and clinical implications. Anal. Chim. Acta [Online] 2019, 1089, 1-18. doi: 10.1016/j.aca.2019.08.044 (accessed July 13, 2021).
- Nupur, N; Chhabra, N.; Dash, R.; Rathore, A.S. Assessment of structural and functional similarity of biosimilar products: Rituximab as a case-study. mAbs [Online] 2018, 10, 143-158. https://www.tandfonline.com/doi/full/10.1080/19420862.2017.1402996 (accessed July 7, 2021).
- Zhang, J; Arbault, S; Sojic, N; Jiang, D. Electrochemiluminescence imaging for bioanalysis. Annu. Rev. Anal. Chem. [Online] 2019, 12, 275-95. https://www.annualreviews.org/doi/10.1146/annurev-anchem-061318-115226 (accessed July 7, 2021).